Do Weight Loss Drugs Enable Lousy Eating Habits?
A physician friend of mine who lost 75+ pounds after being prescribed Wegovy for obesity recently confided to me: “It’s so hard for me to remember to eat healthily, since I can basically eat whatever I want now.”
New weight loss drugs could mean the end of the obesity epidemic, suggest headlines from a wide range of well-known publications such as Forbes, The Economist, The Harvard Gazette, and WebMD. Even the perpetual proponents of willpower formerly known as Weight Watchers are getting in on the weight loss drugs game.
Analyses comparing various diets have concluded that the diet a person can stick to is the one that will help them to lose weight. Now that we have drugs like Wegovy that work, at least to some extent (as far as we know) by significantly decreasing appetite, anyone can stick to any diet and still lose weight.
All of this begs the question: Do we need to care about what we eat anymore? Why shouldn’t we have our cake and eat it too– for breakfast, lunch, and dinner?
The short answer is: Unless someone’s only goal is to be ravishingly thin at their own wake, they’ll probably want to consider the many well-established benefits of a healthy diet, beyond weight control. Because a more reasonable goal than slaying that deathbed look is a healthy lifespan, in which case it does matter what we eat, very much so.
Here’s to our health
Longevity in and of itself can be less of a blessing and more of a curse. After all, we all know that if we don’t have our health….
And the numbers are depressing. The vast majority of us are going to first become debilitated and then ultimately die from one or more of these diseases: type 2 diabetes, high blood pressure, heart disease, heart failure, strokes, kidney disease, cancer. We’ve all seen friends, neighbors and relatives suffer from these slow killers.
So, it’s not about living a long life. Healthy lifespan, and its snappy equivalent “healthspan”, means living disease- and debility-free for as long as possible. And that should be everyone’s goal.
As a physician with a personal family history of chronic disease, I’m keenly interested and invested in making the concept of a healthy lifespan my own reality. Dementia, diabetes, heart disease, kidney disease, and neuropathy have critical risk factors in common, and diet is one of the most important.
But wait — what about weight?
What we eat is not the only factor behind these diagnoses, though. Obesity has long been associated with chronic disease, in particular diabetes and cardiovascular diseases. Studies have shown that people with overweight also have a higher burden of disease as they age, as compared to normal weight individuals. Maybe successfully treating overweight and obesity with drugs is enough to lower these risks?
Evidence does suggest that weight loss drugs help lower certain risks in certain people. A study published in the New England Journal of Medicine showed that people with diabetes who were treated with Ozempic (the version of semaglutide approved for diabetes) had significantly fewer heart attacks and strokes than those who were treated with placebo.
In addition, a recently published study in the journal Diabetes reported that people with obesity being treated with once-weekly Wegovy (the version of semaglutide approved for obesity) had an estimated almost 60% lower risk of developing type 2 diabetes.
Wow, almost 60% reduced risk! What else could possibly be that effective?
Oh, right — a healthy diet and lifestyle.
A massive study called the Diabetes Prevention Program enrolled almost 4,000 people at risk for type 2 diabetes and gave them either a 24-week diet and lifestyle intervention, a medication (Glucophage,the brand name for oral diabetes medication metformin), or a placebo (a fake pill). After three years, people in the diet and lifestyle group had a 58% lower risk of developing type 2 diabetes than the placebo group (and the metformin group had a 31% lower risk, which is also nothing to sniff at). These participants were followed over time, and even after 10 years, the diet and lifestyle group had a 34% lower risk of developing diabetes compared to placebo. That loooong-term study is very well-known, and the CDC adapted the diet and lifestyle program for the masses; for those with prediabetes, it is often covered by insurance, even.
But are diet and lifestyle approaches alone realistic for people?
On the other hand, from my years as a diet-and-lifestyle-focused physician in practice, I know that these approaches alone have never been enough for many people to sustainably and positively impact their health over the long haul.
But consider the risks and side effects of a drug (and I work in the biopharma industry, now) versus a healthy diet. The risks and negative side effects of the new weight loss drugs can include a lot of things, like “nausea, diarrhea, vomiting, constipation, stomach pain, headache” and a number of other things in very small print on that thin white paper that comes in the box. With a healthy diet, however, one is more likely to have benefits and good side effects beyond weight loss.
Gosh, choosing between drugs and diet could be difficult!
But maybe we don’t have to choose?
Drugs vs diet: Can we do both?
One thing we are learning from our experience with weight loss drugs is that they can be extremely effective where nothing else has ever been — not only for weight loss, but also for helping people stick to a healthful diet.
There is evidence to suggest that drugs plus diet could be the best choice for many people. Combining Saxenda (the weight loss version of liraglutide) with a diet and lifestyle intervention has been studied and the results published in the New England Journal of Medicine; as seems intuitive, the combination is significantly more effective for maintenance of weight loss at one year than either approach alone.
In a recent article for the Journal of the American Medical Association, longtime nutrition researcher Dariush Mozaffarian suggests “a new paradigm of initial, staged GLP-1 agonist treatment supported by long-term lifestyle programming”. This combines the dual prescriptions of weight loss drugs with nutrition and lifestyle interventions, much as that Saxenda study did. In his vision, in order to save costs, the drugs can be prescribed in a staged or intermittent fashion; and in order to overcome the structural barriers to healthy diet and lifestyle that many face, these could be prescribed as well, as is already being done in many Food is Medicine programs across the country.
The benefits of combining both likely go far beyond weight loss and weight loss maintenance. We all have genetic tendencies that are influenced by other factors, like what we eat and what we do. This is epigenetics, the field that is often described as where DNA meets diet and lifestyle.
These genetic tendencies can include inherited risks for chronic diseases, like diabetes, heart disease, strokes, dementia, many cancers including lung and colon cancer… Basically, what we eat and how we live can tip the scale in one direction or the other.
Where diet is concerned, it’s super-complicated but pretty clear: bioactive phytochemicals and macronutrients in our diet impact everything in the body from the gut microbiome to the vasculature to the immune system, impacting our risk of developing type 2 diabetes, heart attacks, strokes, dementia, depression, cancer, fractures, and more.
So, what should we eat?
Regardless if we’re using weight loss drugs or not, if we want to keep our body and brain as fit as possible for as long as possible (and we should) then we should eat healthily. But what does that mean exactly? Well, large and respectable studies have concluded that a largely plant-based dietary pattern that is low in animal foods, sugary drinks, snacks and desserts, refined grains, potatoes, and fruit juices is strongly associated with a lower risk of heart disease, strokes, cancer, and basically death from any cause.
Note that “strongly associated” is as strong as conclusions can get when we’re talking about nutrition research, since one can’t exactly lock study participants up, randomize them to receive different diets, control for all possible confounding factors, and observe their health outcomes over decades… that would be impractical, and also unethical, given the weight of the research we do have from a wide range of studies from intelligent observation like The Blue Zones to randomized, prospective trials like PREDIMED, and many in-between.
The American Heart Association’s Dietary Guidance to Improve Cardiovascular Health cites this mountain of evidence when it emphasizes “the importance of dietary patterns beyond individual foods or nutrients” — in other words, a “heart-healthy dietary pattern”.
Respectable guideline-issuing organizations agree: “A healthy diet includes increased consumption of fruits, vegetables, whole grains, fat-free or low-fat dairy, lean proteins, and oils; and limited consumption of foods and beverages with high sodium levels, saturated or trans fats, and added sugars” (as states the U.S, Preventive Services Task Force, quoting the U.S. Department of Health and Human Services, both of these being important evidence- observant guidance-delivering governmental agencies).
How do we know if we’re eating healthily enough?
Given the critical importance of diet for multiple health outcomes, one would think that healthcare providers would be assessing the quality of their patient’s diet at every preventive-focused annual physical. But this is America, and the healthcare system isn’t designed to be health-promoting…yet.
As it is now, it’s not feasible for healthcare providers to quickly, easily and accurately assess the quality of their patient’s diet in an office visit. There are numerous barriers, including lack of time, training, and/or appropriate tools. I’ll just put it out there that when I was in clinical practice at a well-known academic medical center, I was involved with a research group that developed and validated a brief questionnaire designed to solve this problem. We published that research open access in The Journal of the Academy of Nutrition and Dietetics, along with the questionnaire that can quickly, easily and accurately assess the quality of a person’s diet. Here it is:
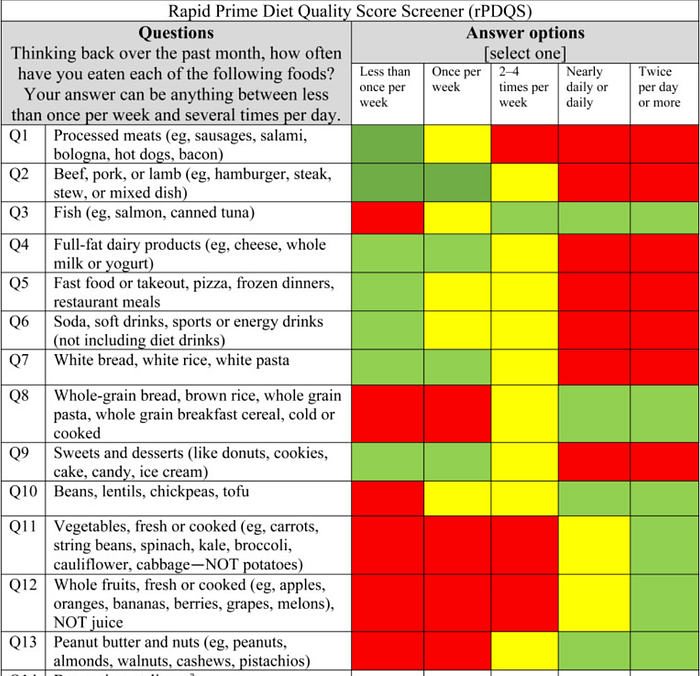
The idea is that the questionnaire would be online in black and white; once completed, the traffic-light colors would emerge, showing patient and provider what’s good (green), borderline (yellow), and potentially harmful (red).
Better living through chemistry…AND nutrition
The conclusion here is, it’s clear what a healthy dietary pattern looks like. Regardless of whether we’re on weight loss drugs or not, if we care about our healthspan, we should care about what we eat. What we nourish our bodies with matters.
Source: https://medium.com/wise-well/do-weight-loss-drugs-enable-lousy-eating-habits-defdeb62fe2b

